Peripheral Arterial Occlusive Disease
What is Peripheral Arterial Occlusive Disease?
Risk Factors:
- Smoking
- High blood pressure
- Diabetes
- Kidney failure
- Obesity
- Age/Gender - more common in males than females
- Lack of exercise
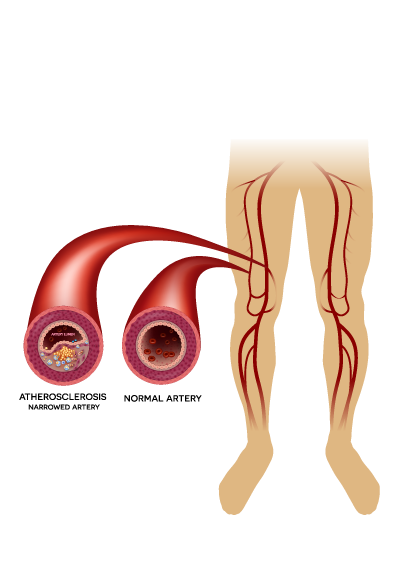
- Family history of atherosclerosis (narrowing of the artery due to buildup of plaque)
Signs & Symptoms:
- Varies depending on the extent/severity of vessel narrowing
- Some people with PAD may not have any symptoms at all
Diagnostic Studies:
- Lower extremity arterial ultrasound- this is a simple study to measure the blood flow to your leg or feet and identify narrowing's in your arteries.
- Diagnostic lower extremity angiogram- This is a minimally invasive study done with the use of a contrast dye, x-rays to visualize the blood flow through the arteries and to identify narrowing's or blockages. This study is more reliable than an ultrasound but cannot be used on a routine basis. The need is determined based on your symptoms by your vascular surgeon.
Claudication
When the blood flow to the legs is reduced the amount of oxygen delivered to the muscles and tissues also reduces. So, when a person walks faster than usual there is more demand for oxygen but the blood vessel is unable to deliver oxygen-rich blood due to the narrowing or blockage in the artery. This causes the muscles to ache. The pain initially resolves when you take short breaks. This is called claudication.
Chronic Limb Threatening Ischemia
As the disease progresses you will start noticing pain even with walking very short distances or with minimal exertion and even at rest. Pain at rest is called rest pain and can lead to limb loss. Rest pain is worse when you elevate your leg and pain improves when the leg is lowered below the heart level.
Over a period of time, the decrease in the oxygen-rich blood flow to the lower leg can cause your skin to become thin, pale with hair loss or thinning, distal legs and feet may feel cold, you could also have non-healing ulcers, infections, or even gangrene (death of a part of the tissue due to lack of oxygen), and it puts you at high risk for limb loss/amputations.
Acute Limb Threatening Ischemia
When there is a sudden loss of blood supply to the lower limbs due to a traveling blood clot or an aneurysm (dilated artery) which has clotted or because of occlusion of a previously placed bypass graft or stent or buildup and occlusion due to plaque at a certain part of the artery it can lead to the risk for immediate limb loss/amputation. It can cause severe pain in the legs, discoloration of the foot or toes ranging from blue to black, sensory loss of the toes/foot, muscle weakness, and rest pain.
Treatments for PAD
The best treatment option for you can be discussed and determined together with your vascular surgeon.
Medical Treatment
No medical therapy can remove the plaque that is already formed in the walls of your arteries, but it can help prevent more deposition of plaque in your arteries and maintain the blood flow to your legs. Medical treatments include maintaining normal blood pressure, blood sugar levels, managing your cholesterol levels, exercising regularly, and stop smoking. If you have kidney disease/diabetes/known heart disease your chances of progression of plaque formation in your arteries are higher.
Smoking is an important risk factor- The nicotine in cigarettes constricts your arteries and causes damage to the walls of the arteries which can lead to deposition of plaque, weakens arterial walls and increases the rate at which plaque builds up in your arteries, and reduces the flow of oxygenated blood which causes symptoms. Stopping smoking is very important to prevent the worsening of your arterial disease and to improve and maintain the oxygenated blood flow to your legs.
Certain medications can be used to help reduce the progression of plaque formation in your arteries and can also improve the pain in your legs with walking. This needs to be discussed with your vascular surgeon.
Surgical Treatment
Open Surgery:
It is a surgical procedure done to reroute the blood supply around a blocked artery in your legs. A natural or synthetic graft is used to reroute the blood around the blocked artery. The graft can be one of your long veins in the legs or artificial arteries made from synthetic materials.
Endarterectomy:
It is the surgical removal of the plaque from the artery while keeping the wall of the artery intact.
With an open bypass surgery or endarterectomy, it involves a hospital stay up to 3-5 days post operatively and a longer recovery time but still can be a good option in terms of lasting results.
Endovascular Surgery:
This is a minimally invasive procedure done to treat narrowing or occlusions in your arteries that were identified with the ultrasound or a diagnostic angiogram to help improve the oxygenated blood flow to your legs. This is a minimally invasive procedure. A long flexible tube called a catheter is inserted through a small cut in your groin or arm and the catheter is guided under ultrasound and x-ray guidance to the artery/blood vessel that is to be treated. A contrast dye is injected through this catheter and the area to be treated is identified and treated with different techniques.
This procedure requires minimal recovery time, you are able to go home the same day if there are no complications.
Techniques used during the angiogram to treat diseased arteries
- Balloon Angioplasty – During this procedure, the doctor makes a small puncture through your skin and inserts a long tube called a catheter and threads a small deflated balloon to the area of the artery which is narrowed and then inflates the balloon to open the narrow or blocked part of the artery.
- Stent Implantation – The doctor can also use a stent along with the balloon to keep the narrowed or blocked artery open. The stent is a small metal mesh tube that helps to keep the artery open. The doctor will thread the stent through a catheter to the narrowed or blocked artery and open it up with a small balloon. The stent stays in the artery permanently.
- Atherectomy – It is a procedure done by using a small mechanically driven cutting device on the end of the catheter to cut or shave away plaque. It can be used alone or along with balloon angioplasty and stenting.
